You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Just had a PRP injection in the rotator cuff today.
- Thread starter undecided
- Start date
I am not a teenager so I have high hopes....thxBest wishes!
My wife and I respond very well to PRP treatments. My teenage kids, not so much.
Has anyone had this particular reaction?
First 2 days, the injection site was quite sore but the baseline pain had diminished.
On the 4th day I made a quick arm movement that resulted in a sharp pain. That night (last night) I had throbbing pain in the shoulder which necessitated the ingestion of tylenol to resolve.
Today ( the 5th day ) is still not as good as the 1st and 2nd days. I do have occasional deep throbbing pain.
Is this normal?
First 2 days, the injection site was quite sore but the baseline pain had diminished.
On the 4th day I made a quick arm movement that resulted in a sharp pain. That night (last night) I had throbbing pain in the shoulder which necessitated the ingestion of tylenol to resolve.
Today ( the 5th day ) is still not as good as the 1st and 2nd days. I do have occasional deep throbbing pain.
Is this normal?
pats300zx1
New User
I am getting a PRP injection next Thursday in my elbow for my TE. Hoping this helps in clearing it up.
I may do that as well, depending on how well the shoulder does. Although I had TE last August and have not hit a tennis ball since january, when I grab the flexbar and do a taylor twist, I do feel twinges in the lateral epicondyle. I don't think it ever healed properly.I am getting a PRP injection next Thursday in my elbow for my TE. Hoping this helps in clearing it up.
Another update, shoulder was throbbing last night while watching TV, very discouraging.
I went to bed thinking I will have to get up in the middle of the night for tylenol but weirdly enough, I slept through the night with zero pain.
Is it possible that the throbbing was the start of healing?
I went to bed thinking I will have to get up in the middle of the night for tylenol but weirdly enough, I slept through the night with zero pain.
Is it possible that the throbbing was the start of healing?
travlerajm
Talk Tennis Guru
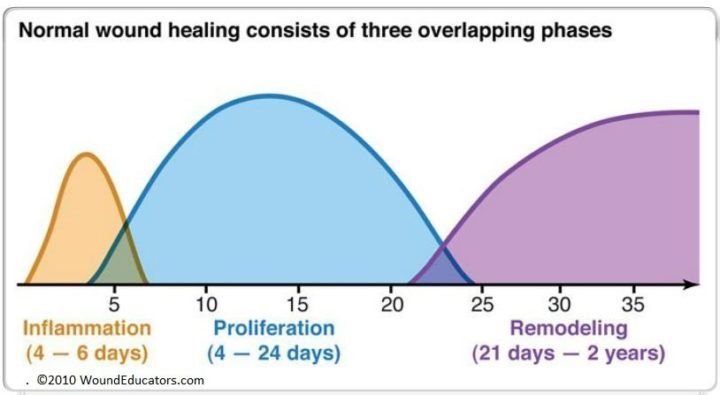
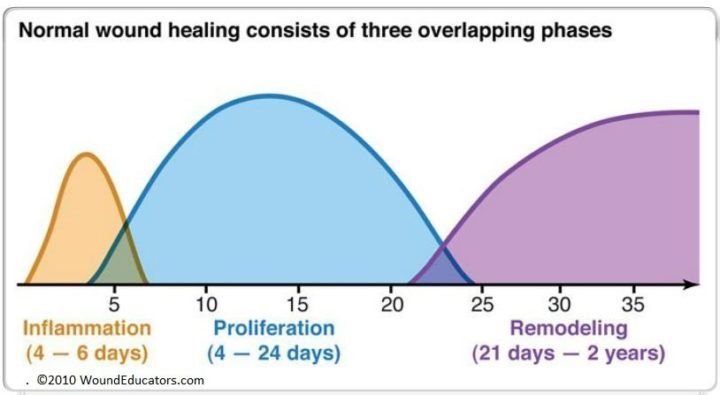
Inflammatory stage of healing peaks 3-5 days post.Another update, shoulder was throbbing last night while watching TV, very discouraging.
I went to bed thinking I will have to get up in the middle of the night for tylenol but weirdly enough, I slept through the night with zero pain.
Is it possible that the throbbing was the start of healing?
Phases of Wound Healing- Part 1
Wound healing proceeds in a relatively organized fashion, following three processes that overlap- inflammation, proliferation and maturation/remodeling (some sources will describe this process as four phases breaking the inflammation process into hemostasis and inflammation). How
Thx, that makes sense. Most prp articles say the swelling/pain goes down after 24-48hrs which it did for me. Then this throbbing started.Inflammatory stage of healing peaks 3-5 days post.
Phases of Wound Healing- Part 1
Wound healing proceeds in a relatively organized fashion, following three processes that overlap- inflammation, proliferation and maturation/remodeling (some sources will describe this process as four phases breaking the inflammation process into hemostasis and inflammation). Howwoundeducators.com
Update: 9 days in, pain in Supraspinatus area has disappeared. I had 2 subluxations while sleeping 2 nights ago that woke me up and really probably set me back a couple of days as far as pain goes because pain had completely disappeared that day. Not sure what that's all about. I hadn't had one since the early days of the injury. Shoulder is still stiff (not from pain, just stiff) and ROM is still non-existent as far as external rotation goes. Started light rotator cuff exercises yesterday, stretching, strengthening and stabilizing. If this continues to improve this well, I will do more PRP.
yossarian
Professional
Update: 9 days in, pain in Supraspinatus area has disappeared. I had 2 subluxations while sleeping 2 nights ago that woke me up and really probably set me back a couple of days as far as pain goes because pain had completely disappeared that day. Not sure what that's all about. I hadn't had one since the early days of the injury. Shoulder is still stiff (not from pain, just stiff) and ROM is still non-existent as far as external rotation goes. Started light rotator cuff exercises yesterday, stretching, strengthening and stabilizing. If this continues to improve this well, I will do more PRP.
you’ve had subluxations? Do you have a history of dislocations?
I had one dislocation on same shoulder 25 yrs ago. I've had about 10 subluxations since january. Always while sleeping.you’ve had subluxations? Do you have a history of dislocations?
p.s. I paid more attention last night. Lying flat on my back, just having the pillow get under behind the shoulder and pushing it up an inch or so triggers the feeling that it may subluxate.
Last edited:
Raul_SJ
G.O.A.T.
I had one dislocation on same shoulder 25 yrs ago. I've had about 10 subluxations since january. Always while sleeping.
What is your diagnosis? Rotator cuff tear? Tendonitis?
Copying from the report:What is your diagnosis? Rotator cuff tear? Tendonitis?
"
Moderate grade partial thickness tear along the anterior fibers of the supraspinatus insertion, possibly noncommunicating.
Findings concerning for a posterior labral tear extending from proximally 7-9 o'clock.
Mild inflammatory changes compatible with adhesive capsulitis.
"
Say Chi Sin Lo
G.O.A.T.
Copying from the report:
"
Moderate grade partial thickness tear along the anterior fibers of the supraspinatus insertion, possibly noncommunicating.
Findings concerning for a posterior labral tear extending from proximally 7-9 o'clock.
Mild inflammatory changes compatible with adhesive capsulitis.
"
Uhhh... I am not sure why you are doing PRP, or other stem cell / regenerative therapy, unless your sports medicine doctor/surgeon recommended it. It sounds like you have structural defects that require surgical intervention. Either in the form of repairing the supraspinatus tendon and the posterior labral, or shaving off the torn/fraying end so you have one continuous tissue. Maybe my science is out of date but I am under the impression that regenerative therapies aid in mostly cartilage tissue, I am not sure how much it's doing for your supraspinatus defect?
I had very similar diagnosis when a 2nd surgery was required
- partial thickness tear of my supraspinatus - repaired
- posterior labral tear - repaired
- I was 22 years old at the time. Rehab sucked and I would not return to full strength (tennis wise) for another 2 years.
You may be right but I am noticing significant changes with the PRP. It has calmed down the pain in the supraspinatus enough where I was able to resume PT where before I could not. I actually question everything in this MRI as my symptoms have changed over time. It all started with intense sharp stabbing pains when I hit a tennis ball or if I really stretched my arm out. I still had full range of motion. Got a cortizone shot into the supra area as that was the suspect for tendonitis (My manual physical exam did not show evidence of tears, I was quite strong in all angles). 2 weeks later pain persisted so I Had the MRI. THen I started PT but that got interrupted by Covid. During the covid shut down, symptoms changed. I did not have the sharp stabbing pains anymore but range of motion really went down dramatically, external rotation basically shut down. Upon resumption of PT, the supraspinatus just hurt too much to be able to do anything productive, so the PT and a person that had had PRP in the supra area that was doing PT at a time convinced me to ask my doctor about and he agreed to do it.Uhhh... I am not sure why you are doing PRP, or other stem cell / regenerative therapy, unless your sports medicine doctor/surgeon recommended it. It sounds like you have structural defects that require surgical intervention. Either in the form of repairing the supraspinatus tendon and the posterior labral, or shaving off the torn/fraying end so you have one continuous tissue. Maybe my science is out of date but I am under the impression that regenerative therapies aid in mostly cartilage tissue, I am not sure how much it's doing for your supraspinatus defect?
I had very similar diagnosis when a 2nd surgery was required
- partial thickness tear of my supraspinatus - repaired
- posterior labral tear - repaired
- I was 22 years old at the time. Rehab sucked and I would not return to full strength (tennis wise) for another 2 years.
Anyway, I am exactly 2 weeks into it and I did see changes. I am now able to perform most rehab exercises with no pain, I am improving my ROM. One negative/questionable thing is that I do have bouts of dull pain but they are located further forward than where the supraspinatus is. My doc thinks its the labrum tear area. I also have bouts of sharp pain at night but that's normal for this I think.
BTW, PRP has shown improvements to partial tendon tears, the science is not 100% conclusive but there are lot of anecdotal evidence that it works about 50-60% of the time depending on the tear. I've even seen cases of PRP into the labrum tear. If it's only frayed and not detached, it can even work for that.
Update:
A little over 2 weeks since the PRP and if you asked me 4-5 days ago, I would have said surgery is inevitable.
I had reduced strength (50% of good shoulder and pain in certain movements). Range of motion poor.
If you asked me yesterday I would have said OMG, it's getting healed.
Strength was up to about 80% of good shoulder and no pain in any direction. Range of motion still poor but better, I can put hand in back pocket now.
If you ask me today I will give you a shrug.
Haven't checked the strength yet but I did a quick move like a swipe of the bottom of my foot while standing to flick something off, my hand barely encountered any force and still got a debilitating sharp pain in the same spot as before. Caught me totally by surprise since it had been so good the last few days.
A little over 2 weeks since the PRP and if you asked me 4-5 days ago, I would have said surgery is inevitable.
I had reduced strength (50% of good shoulder and pain in certain movements). Range of motion poor.
If you asked me yesterday I would have said OMG, it's getting healed.
Strength was up to about 80% of good shoulder and no pain in any direction. Range of motion still poor but better, I can put hand in back pocket now.
If you ask me today I will give you a shrug.
Haven't checked the strength yet but I did a quick move like a swipe of the bottom of my foot while standing to flick something off, my hand barely encountered any force and still got a debilitating sharp pain in the same spot as before. Caught me totally by surprise since it had been so good the last few days.
Well, mine have been hurting for 6 months with no sign of healing and I saw changes 10 days after the PRP so it can't be a coincidence.PRP did heal 3 of my rotator partial tears. The doc missed treating a fourth so that one is the control tear. The "control tear" did not heal. Even with PRP my healing time was 8-10 months. Long-term physical therapy (on your own) is important.
Yes, I am doing PT. I think I overdid it though, I increased the theraband strength too quickly and my shoulder was achy yesterday.
I am going to dial it back.
Were your tears on different tendons?
Update, I had a 2nd opinion from a different doc today. He said he has not seen good PRP results for the shoulder, he had used them post-operatively. He does use them for other injuries like knees.
He said my biggest problem right now is the frozen shoulder. He wasn't too worried about the tears. He said it's possible the symptoms I experienced early on were the onset of frozen shoulder and not the result of the MRI shown tears.
He said my biggest problem right now is the frozen shoulder. He wasn't too worried about the tears. He said it's possible the symptoms I experienced early on were the onset of frozen shoulder and not the result of the MRI shown tears.
Say Chi Sin Lo
G.O.A.T.
Update, I had a 2nd opinion from a different doc today. He said he has not seen good PRP results for the shoulder, he had used them post-operatively. He does use them for other injuries like knees.
He said my biggest problem right now is the frozen shoulder. He wasn't too worried about the tears. He said it's possible the symptoms I experienced early on were the onset of frozen shoulder and not the result of the MRI shown tears.
Not that I want to burst your bubble, because an individual's perception often trumps scientific data. (I mean, if it feels better than it feels better to that person, simple as that)
But I can post a lecture video from UCSF suggesting PRP has minuscule effects. Would you be interested in the lecture video?
Sure, I've seen countless videos. A lot say PRP is bunk as far as the shoulder is concerned because there are no 'good' studies on it yet, most studies are too small or don't have a true control, etc, etc, but then you have a lot of anecdotal evidence that it does do something positive.Not that I want to burst your bubble, because an individual's perception often trumps scientific data. (I mean, if it feels better than it feels better to that person, simple as that)
But I can post a lecture video from UCSF suggesting PRP has minuscule effects. Would you be interested in the lecture video?
yossarian
Professional
frozen shoulder
That's unfortunately a self-limiting condition. It will resolve within a certain timeframe as it progresses through its phases. PT can help you, or a steroid injection if caught early, but ultimately it's going to have to run its course
Yes, that's what I've read and what the doctor said. Doctor agreed with me that it's very possible that the early symptoms I had (pain, pain, pain) were not due to the tears shown in the MRI but maybe due to the Stage 1 of the frozen shoulder. It's very possible the tears are asymptomatic but we can't know until the frozen shoulder thaws.That's unfortunately a self-limiting condition. It will resolve within a certain timeframe as it progresses through its phases. PT can help you, or a steroid injection if caught early, but ultimately it's going to have to run its course
Raul_SJ
G.O.A.T.
Yes, that's what I've read and what the doctor said. Doctor agreed with me that it's very possible that the early symptoms I had (pain, pain, pain) were not due to the tears shown in the MRI but maybe due to the Stage 1 of the frozen shoulder. It's very possible the tears are asymptomatic but we can't know until the frozen shoulder thaws.
This is a test for True Frozen Shoulder. 96% sensitivity.
You may have Pseudo Frozen Shoulder.
Patients under anaesthesia are often able to gain
range of motion. If so, that means there is a huge psycho somatic component!
Last edited:
This is a test for True Frozen Shoulder. 96% sensitivity.
You may have Pseudo Frozen Shoulder.
Patients under anaesthesia are often able to gain
range of motion. If so, that means there is a huge psycho somatic component!
Yowzers! All 3 points hurt on me with the coracoid the worst.
"If so, that means there is a huge psycho somatic component"
Uh, it sounds like you're surprised at this. There's ALWAYS a psycho somatic component to pain and injury. Always.
Raul_SJ
G.O.A.T.
Yowzers! All 3 points hurt on me with the coracoid the worst.
"If so, that means there is a huge psycho somatic component"
Uh, it sounds like you're surprised at this. There's ALWAYS a psycho somatic component to pain and injury. Always.
Not clear of the implications of the study.
If a patient with frozen shoulder can only abduct 50% of normal motion, but under anaesthesia exhibits far greater ROM, that means he does not have true frozen shoulder. He can safely push himself more in his stretching sessions? But it is strange that they say all patients had greater ROM under anaesthesia.
A true frozen shoulder ROM would not improve under anaestheseia.
Hollman 2015, did a study on the amount of active muscle guarding in patients suspected of a frozen shoulder and found that all patients experienced a huge increase in passive abduction while under anesthesia.
This means that the loss of range of motion in frozen shoulder can not only be explained by a true capsular contracture alone but that active stiffness or muscle guarding can play a huge role as well.
Last edited:
The doc palpated those areas.This is a test for True Frozen Shoulder. 96% sensitivity.
You may have Pseudo Frozen Shoulder.
Patients under anaesthesia are often able to gain
range of motion. If so, that means there is a huge psycho somatic component!
I don't think you can safely push as then you will damage the muscles and tendons that are fighting against you. For example, yesterday I added specific frozen shoulder stretches to my daily exercise regiment. Man, I won't do that again, let it be and thaw by itself. I had some much pain at night. The doc did say that If I do them I will be in pain and will have to take 2 Aleve per day to control the pain.Not clear of the implications of the study.
If a patient with frozen shoulder can only abduct 50% of normal motion, but under anaesthesia exhibits far greater ROM, that means he does not have true frozen shoulder. He can safely push himself more in his stretching sessions? But it is strange that they say all patients had greater ROM under anaesthesia.
A true frozen shoulder ROM would not improve under anaestheseia.
Hoffman 2015, did a study on the amount of active muscle guarding in patients suspected of a frozen shoulder and found that all patients experienced a huge increase in passive abduction while under anesthesia.This means that the loss of range of motion in frozen shoulder can not only be explained by a true capsular contracture alone but that active stiffness or muscle guarding can play a huge role as well.
Raul_SJ
G.O.A.T.
I don't think you can safely push as then you will damage the muscles and tendons that are fighting against you. For example, yesterday I added specific frozen shoulder stretches to my daily exercise regiment. Man, I won't do that again, let it be and thaw by itself. I had some much pain at night. The doc did say that If I do them I will be in pain and will have to take 2 Aleve per day to control the pain.
The controversy is whether those moderate stretches will quicken the recovery. Some Doctors will advise the stretching if you can tolerate the pain. Others will say that it will resolve on its own without stretching... I am thinking that stretching during the thawing phase might quicken the thawing. Or at least will not do any harm... So if there is a chance, might as well do the stretches.
The doc palpated those areas.
If there was pain, that means it is likely true frozen shoulder.
What was the result?
No pain BUT when my shoulder is not feeling well there is some pain.The controversy is whether those moderate stretches will quicken the recovery. Some Doctors will advise the stretching if you can tolerate the pain. Others will say that it will resolve on its own without stretching... I am thinking that stretching during the thawing phase might quicken the thawing. Or at least will not do any harm... So if there is a chance, might as well do the stretches.
If there was pain, that means it is likely true frozen shoulder.
What was the result?
p.s. If this is psychosomatic it must be the most screwed up psycho sh1t ever because when the arm reaches the 'end' it feels as if it runs against a solid block of material like bone. Pushing further only results in me moving my whole right side along with the arm as a solid structure.
Raul_SJ
G.O.A.T.
No pain BUT when my shoulder is not feeling well there is some pain.
p.s. If this is psychosomatic it must be the most screwed up psycho sh1t ever because when the arm reaches the 'end' it feels as if it runs against a solid block of material like bone. Pushing further only results in me moving my whole right side along with the arm as a solid structure.
The video talks about "pseudo" frozen shoulder vs true frozen shoulder and "active muscle guarding" and patients exhibiting greater ROM under anaesthesia... Video is not clear what % of cases are true vs pseudo.
Here is a diffetrent example of pseudo frozen shoulder. Not psychosomatic but not true Adhesive Capsulitis:
A true Frozen Shoulder is due to Adhesive Capsulitis, which is a thickening of the joint capsule in the shoulder. This can be for many reasons and is confirmed by specialist assessment and imaging.
Unfortunately, when we see a restriction in shoulder movement we often leap to conclusions and assume it's "Frozen".
But if we take a thorough history, utilise a thorough palpation and movement screen; we can often stumble upon breadcrumbs which will lead us to a solution.
Recently, I had a client come to see me for a "Frozen" Shoulder. He had been diagnosed 3 months previous but without imaging. His right shoulder had been restricted for around 6 months.
On taking a history, the client had suffered no direct injury to the shoulder it had just developed over a few months. The main related trauma he had received had been due to his career as a helicopter pilot in the Forces. In this job he had to wear an extremely heavy helmet, laden with equipment, as he flew the helicopter which he controlled via a stick control with his right arm.
Palpation and motion assessment indicated that the problem was actually related to the neck and an instability there. This was creating instability in the Right Side Posterior Scalene (a neck muscle), causing a constant "lifting" of the First Rib. This then created instability in the Serratus Anterior (Scapula muscle) which shares an attachment at the First Rib but also attaches to the Scapula (shoulder blade).
The body had counteracted instability at the Scapula by Facilitating (Neurologically strengthening) the Latissimus Dorsi Muscle and then Inhibiting (Neurologically weakening) the Supraspinatus.
This is what had created the "Frozen Shoulder".
By correcting the Posterior Scalene to Serratus Anterior dysfunction, mobilising the Latissimus Dorsi and strengthening the Supraspinatus we managed to restore full movement to the shoulder within 3 visits.

Frozen Shoulder - is it really?
A true Frozen Shoulder is due to Adhesive Capsulitis, which is a thickening of the joint capsule in the shoulder. This can be for many reasons and is confirmed by specialist assessment and imaging. Unfortunately, when we see a restriction in shoulder movement we often leap to conclusions and...
OK, I will play....If indeed there are causes like the described here why would they all resolve spontaneously within the timeframe prescribed for adhesive capsulitis. BTW, my original MRI did mention capsular inflammation consistent with early stage Adhesive Capsulitis. Of course, everything in the MRI was 'possible this', 'possible that'. Only thing that had conviction was the supraspinatus partial tear.The video talks about "pseudo" frozen shoulder vs true frozen shoulder and "active muscle guarding" and patients exhibiting greater ROM under anaesthesia... Video is not clear what % of cases are true vs pseudo.
Here is a diffetrent example of pseudo frozen shoulder. Not psychosomatic but not true Adhesive Capsulitis:
A true Frozen Shoulder is due to Adhesive Capsulitis, which is a thickening of the joint capsule in the shoulder. This can be for many reasons and is confirmed by specialist assessment and imaging.Unfortunately, when we see a restriction in shoulder movement we often leap to conclusions and assume it's "Frozen".But if we take a thorough history, utilise a thorough palpation and movement screen; we can often stumble upon breadcrumbs which will lead us to a solution.Recently, I had a client come to see me for a "Frozen" Shoulder. He had been diagnosed 3 months previous but without imaging. His right shoulder had been restricted for around 6 months.On taking a history, the client had suffered no direct injury to the shoulder it had just developed over a few months. The main related trauma he had received had been due to his career as a helicopter pilot in the Forces. In this job he had to wear an extremely heavy helmet, laden with equipment, as he flew the helicopter which he controlled via a stick control with his right arm.Palpation and motion assessment indicated that the problem was actually related to the neck and an instability there. This was creating instability in the Right Side Posterior Scalene (a neck muscle), causing a constant "lifting" of the First Rib. This then created instability in the Serratus Anterior (Scapula muscle) which shares an attachment at the First Rib but also attaches to the Scapula (shoulder blade).The body had counteracted instability at the Scapula by Facilitating (Neurologically strengthening) the Latissimus Dorsi Muscle and then Inhibiting (Neurologically weakening) the Supraspinatus.This is what had created the "Frozen Shoulder".By correcting the Posterior Scalene to Serratus Anterior dysfunction, mobilising the Latissimus Dorsi and strengthening the Supraspinatus we managed to restore full movement to the shoulder within 3 visits.
Raul_SJ
G.O.A.T.
BTW, my original MRI did mention capsular inflammation consistent with early stage Adhesive Capsulitis. Of course, everything in the MRI was 'possible this', 'possible that'. Only thing that had conviction was the supraspinatus partial tear.
Tears are often asymptomatic. This introduces more complexity.
Also, some patients report that Adhesive Capsilutis was very clearly shown in MRI while others report that nothing was shown and the Adhesive Capsilutis was diagnosed clinically.
Raul_SJ
G.O.A.T.
If indeed there are causes like the described here why would they all resolve spontaneously within the timeframe prescribed for adhesive capsulitis.
True Frozen Shoulder (Adhesive Capsulitis) typically takes a year or more to resolve.
In that example, it was resolved within a few visits following the differential diagnosis .
Are you suggesting it would have resolved in a year even if the differential diagnosis was missed?
This is what had created the "Frozen Shoulder".
By correcting the Posterior Scalene to Serratus Anterior dysfunction, mobilising the Latissimus Dorsi and strengthening the Supraspinatus we managed to restore full movement to the shoulder within 3 visits.
Last edited:
yossarian
Professional
The video talks about "pseudo" frozen shoulder vs true frozen shoulder and "active muscle guarding" and patients exhibiting greater ROM under anaesthesia... Video is not clear what % of cases are true vs pseudo.
Here is a diffetrent example of pseudo frozen shoulder. Not psychosomatic but not true Adhesive Capsulitis:
A true Frozen Shoulder is due to Adhesive Capsulitis, which is a thickening of the joint capsule in the shoulder. This can be for many reasons and is confirmed by specialist assessment and imaging.Unfortunately, when we see a restriction in shoulder movement we often leap to conclusions and assume it's "Frozen".But if we take a thorough history, utilise a thorough palpation and movement screen; we can often stumble upon breadcrumbs which will lead us to a solution.Recently, I had a client come to see me for a "Frozen" Shoulder. He had been diagnosed 3 months previous but without imaging. His right shoulder had been restricted for around 6 months.On taking a history, the client had suffered no direct injury to the shoulder it had just developed over a few months. The main related trauma he had received had been due to his career as a helicopter pilot in the Forces. In this job he had to wear an extremely heavy helmet, laden with equipment, as he flew the helicopter which he controlled via a stick control with his right arm.Palpation and motion assessment indicated that the problem was actually related to the neck and an instability there. This was creating instability in the Right Side Posterior Scalene (a neck muscle), causing a constant "lifting" of the First Rib. This then created instability in the Serratus Anterior (Scapula muscle) which shares an attachment at the First Rib but also attaches to the Scapula (shoulder blade).The body had counteracted instability at the Scapula by Facilitating (Neurologically strengthening) the Latissimus Dorsi Muscle and then Inhibiting (Neurologically weakening) the Supraspinatus.This is what had created the "Frozen Shoulder".By correcting the Posterior Scalene to Serratus Anterior dysfunction, mobilising the Latissimus Dorsi and strengthening the Supraspinatus we managed to restore full movement to the shoulder within 3 visits.
Frozen Shoulder - is it really?
A true Frozen Shoulder is due to Adhesive Capsulitis, which is a thickening of the joint capsule in the shoulder. This can be for many reasons and is confirmed by specialist assessment and imaging. Unfortunately, when we see a restriction in shoulder movement we often leap to conclusions and...www.adfitness.biz
this was written by a personal trainer. I’m having difficulty grasping his rationale, and why this person’s passive ROM would be limited in multiple directions (which is a hallmark of adhesive capsulitis)
If his scapula isn’t moving properly, then yeah, active overhead elevation will be impaired. But I cannot understand why this would significantly limit passive ER and IR as well
the only other resource I could find that mentions the scalenes with regard to frozen shoulder refers to thoracic outlet syndrome as a differential dx. You’d expect sensory changes with that
also of note is that the posterior scalene doesn’t even attach to the first rib
Raul_SJ
G.O.A.T.
why this person’s passive ROM would be limited in multiple directions (which is a hallmark of adhesive capsulitis)
If it was true Frozen Shoulder (Adhesive Capsulitis) would we expect a significant increase in ROM under GA??
Results: All patients had significantly more passive shoulder abduction ROM under general anaesthesia compared to ROM measured while awake. The subject with the smallest difference in these two measures achieved an increase of 44° under general anaesthesia (94° awake vs 138° under GA); the subject with the largest demonstrated a 110° increase under general anaesthesia (55° awake vs 165° under GA).
Conclusion(s): This study demonstrated a variable but significant increase in passive ROM under GA in all patients, indicating that passive ROM loss in FS is not be fully explained by a true capsular contracture alone. Passive shoulder abduction ROM assessed in awake patients with FS does not accurately reflect the true available ROM of the affected shoulder. It appears that active stiffness or muscle guarding is a major contributing factor to reduced ROM in patients with FS.
Implications: Most conservative and surgical treatments for FS aim to increase shoulder ROM by stretching or releasing the shoulder capsule. This study demonstrates that at least a subset of patients with a clinical diagnosis of FS do not have significant capsular restriction. Being able to identify these patients is important to be able to implement an appropriate care pathway as alternative treatments addressing pain and active stiffness need to be considered.
Last edited:
Yes, if as suggested, a large portion of frozen shoulder cases are indeed pseudo frozen shoulder, how come they eventually clear up without treatment for the real underlying condition?True Frozen Shoulder (Adhesive Capsulitis) typically takes a year or more to resolve.
In that example, it was resolved within a few visits following the differential diagnosis .
Are you suggesting it would have resolved in a year even if the differential diagnosis was missed?

My doc said he sees the 'adhesive capsulitis' in almost every MRI report. He sees it so much that it's basically ignored.Tears are often asymptomatic. This introduces more complexity.
Also, some patients report that Adhesive Capsilutis was very clearly shown in MRI while others report that nothing was shown and the Adhesive Capsilutis was diagnosed clinically.
Raul_SJ
G.O.A.T.
Yes, if as suggested, a large portion of frozen shoulder cases are indeed pseudo frozen shoulder, how come they eventually clear up without treatment for the real underlying condition?
Maybe the underlying condition and pseudo Frozen Shoulder resolve eventually within a year.
It still does not explain how the differential diagnosis resolved the pseudo shoulder issue in a very short time.
Well, that was one case, which is considered anecdotal. As a sidenote, frozen shoulder describes many conditions one of them being adhesive capsulitis. The terms should not be used interchangeably unless the adhesion is clearly seen in the MRI like you said.Maybe the underlying condition and pseudo Frozen Shoulder resolve eventually within a year.
It still does not explain how the differential diagnosis resolved the pseudo shoulder issue in a very short time.
Raul_SJ
G.O.A.T.
Well, that was one case, which is considered anecdotal. As a sidenote, frozen shoulder describes many conditions one of them being adhesive capsulitis. The terms should not be used interchangeably unless the adhesion is clearly seen in the MRI like you said.
My understanding is that Adhesive Capsulitis is Frozen Shoulder or "true" Frozen Shoulder.
Sometimes Adhesive Capsulitis is clearly shown on MRI as below. Other times MRI is completely normal.
Given that true Frozen Shoulder can be diagnosed clinically without adhesions necessarily showing on MRI, there is some controversy on using the term
Adhesive Capsulitis.

Adhesive Capsulitis.
MRI . All the white is thickness of the capsule.

Last edited:
Couple of quick thoughts:
1. Regarding adhesions and imaging, you have to understand that a lot of times adhesions/restrictions of the connective tissue (fascia) do not show up on modern imaging (MRI, ultrasound, Xray). So you can have a "normal" MRI but still have adhesions in the shoulder. But believe me when it's thick enough to show up on the MRI, you could potentially be in trouble with regards to the frozen shoulder.
2. There's a lot of things going on in the complex shoulder joint. Things have to work just right between multiple joints, muscles have to pass through small spaces and work in unison with each other in order to produce the motion/strength the mind is asking for. Any upset or kink can throw the whole system into haywire. That's why it takes a good clinician to really try to figure out what's really going on. Because yes the term "frozen shoulder" gets thrown out there a lot because it's easy. Kinda like "low back pain". So good on that person in post #34 to really look at his client and figure out truly what was going on.
Too many clinicians rely on the doctors' diagnosis and try to apply a formula that they've learned or read to treat that diagnosis and don't take the time to examine what else may be going on. Then they just wash, rinse and repeat when that person comes into therapy/treatment. And then when that patient/client doesn't get better, they wind up poo-pooing that therapy "Oh, Physical Therapy stinks, it didn't do anything for me", etc...
3. Like I mentioned before, there's ALWAYS a mind-body connection to pain and injury. Some of these "spontaneous" recoveries can happen bc of all of a sudden the mind can "let go" of whatever it's holding onto and allows the muscle guarding to un-guard, so to speak. Some of these subconscious holding patterns can be VERY VERY powerful and strong and no matter what stretch, exercise or manual work you do, it won't make a lick of difference.
Or, like in the example in post #34, the true cause of why the shoulder went into haywire was found and effectively treated. So for example if you pull down on the bottom of your shirt, you can feel the effects of that pull by your collar/neck. So you treat your neck and you treat your neck w/o much improvement. But until you release that pressure from the bottom of your shirt, the collar will not resolve fully. But once you do release that pressure from the bottom, sometimes it's almost instantaneous on how much relief you get at the collar.
1. Regarding adhesions and imaging, you have to understand that a lot of times adhesions/restrictions of the connective tissue (fascia) do not show up on modern imaging (MRI, ultrasound, Xray). So you can have a "normal" MRI but still have adhesions in the shoulder. But believe me when it's thick enough to show up on the MRI, you could potentially be in trouble with regards to the frozen shoulder.
2. There's a lot of things going on in the complex shoulder joint. Things have to work just right between multiple joints, muscles have to pass through small spaces and work in unison with each other in order to produce the motion/strength the mind is asking for. Any upset or kink can throw the whole system into haywire. That's why it takes a good clinician to really try to figure out what's really going on. Because yes the term "frozen shoulder" gets thrown out there a lot because it's easy. Kinda like "low back pain". So good on that person in post #34 to really look at his client and figure out truly what was going on.
Too many clinicians rely on the doctors' diagnosis and try to apply a formula that they've learned or read to treat that diagnosis and don't take the time to examine what else may be going on. Then they just wash, rinse and repeat when that person comes into therapy/treatment. And then when that patient/client doesn't get better, they wind up poo-pooing that therapy "Oh, Physical Therapy stinks, it didn't do anything for me", etc...
3. Like I mentioned before, there's ALWAYS a mind-body connection to pain and injury. Some of these "spontaneous" recoveries can happen bc of all of a sudden the mind can "let go" of whatever it's holding onto and allows the muscle guarding to un-guard, so to speak. Some of these subconscious holding patterns can be VERY VERY powerful and strong and no matter what stretch, exercise or manual work you do, it won't make a lick of difference.
Or, like in the example in post #34, the true cause of why the shoulder went into haywire was found and effectively treated. So for example if you pull down on the bottom of your shirt, you can feel the effects of that pull by your collar/neck. So you treat your neck and you treat your neck w/o much improvement. But until you release that pressure from the bottom of your shirt, the collar will not resolve fully. But once you do release that pressure from the bottom, sometimes it's almost instantaneous on how much relief you get at the collar.
PT has always worked for me in the past for multiple injuries (including shoulder). This is the 1st time that PT did not work but from what I've read PT does not really work on true adhesive capsulitis.Couple of quick thoughts:
1. Regarding adhesions and imaging, you have to understand that a lot of times adhesions/restrictions of the connective tissue (fascia) do not show up on modern imaging (MRI, ultrasound, Xray). So you can have a "normal" MRI but still have adhesions in the shoulder. But believe me when it's thick enough to show up on the MRI, you could potentially be in trouble with regards to the frozen shoulder.
2. There's a lot of things going on in the complex shoulder joint. Things have to work just right between multiple joints, muscles have to pass through small spaces and work in unison with each other in order to produce the motion/strength the mind is asking for. Any upset or kink can throw the whole system into haywire. That's why it takes a good clinician to really try to figure out what's really going on. Because yes the term "frozen shoulder" gets thrown out there a lot because it's easy. Kinda like "low back pain". So good on that person in post #34 to really look at his client and figure out truly what was going on.
Too many clinicians rely on the doctors' diagnosis and try to apply a formula that they've learned or read to treat that diagnosis and don't take the time to examine what else may be going on. Then they just wash, rinse and repeat when that person comes into therapy/treatment. And then when that patient/client doesn't get better, they wind up poo-pooing that therapy "Oh, Physical Therapy stinks, it didn't do anything for me", etc...
3. Like I mentioned before, there's ALWAYS a mind-body connection to pain and injury. Some of these "spontaneous" recoveries can happen bc of all of a sudden the mind can "let go" of whatever it's holding onto and allows the muscle guarding to un-guard, so to speak. Some of these subconscious holding patterns can be VERY VERY powerful and strong and no matter what stretch, exercise or manual work you do, it won't make a lick of difference.
Or, like in the example in post #34, the true cause of why the shoulder went into haywire was found and effectively treated. So for example if you pull down on the bottom of your shirt, you can feel the effects of that pull by your collar/neck. So you treat your neck and you treat your neck w/o much improvement. But until you release that pressure from the bottom of your shirt, the collar will not resolve fully. But once you do release that pressure from the bottom, sometimes it's almost instantaneous on how much relief you get at the collar.
yossarian
Professional
Couple of quick thoughts:
1. Regarding adhesions and imaging, you have to understand that a lot of times adhesions/restrictions of the connective tissue (fascia) do not show up on modern imaging (MRI, ultrasound, Xray). So you can have a "normal" MRI but still have adhesions in the shoulder. But believe me when it's thick enough to show up on the MRI, you could potentially be in trouble with regards to the frozen shoulder.
2. There's a lot of things going on in the complex shoulder joint. Things have to work just right between multiple joints, muscles have to pass through small spaces and work in unison with each other in order to produce the motion/strength the mind is asking for. Any upset or kink can throw the whole system into haywire. That's why it takes a good clinician to really try to figure out what's really going on. Because yes the term "frozen shoulder" gets thrown out there a lot because it's easy. Kinda like "low back pain". So good on that person in post #34 to really look at his client and figure out truly what was going on.
Too many clinicians rely on the doctors' diagnosis and try to apply a formula that they've learned or read to treat that diagnosis and don't take the time to examine what else may be going on. Then they just wash, rinse and repeat when that person comes into therapy/treatment. And then when that patient/client doesn't get better, they wind up poo-pooing that therapy "Oh, Physical Therapy stinks, it didn't do anything for me", etc...
3. Like I mentioned before, there's ALWAYS a mind-body connection to pain and injury. Some of these "spontaneous" recoveries can happen bc of all of a sudden the mind can "let go" of whatever it's holding onto and allows the muscle guarding to un-guard, so to speak. Some of these subconscious holding patterns can be VERY VERY powerful and strong and no matter what stretch, exercise or manual work you do, it won't make a lick of difference.
Or, like in the example in post #34, the true cause of why the shoulder went into haywire was found and effectively treated. So for example if you pull down on the bottom of your shirt, you can feel the effects of that pull by your collar/neck. So you treat your neck and you treat your neck w/o much improvement. But until you release that pressure from the bottom of your shirt, the collar will not resolve fully. But once you do release that pressure from the bottom, sometimes it's almost instantaneous on how much relief you get at the collar.
do you really think posterior scalene tightness could cause a cascade that presents as frozen shoulder? I could see neurogenic symptoms due to compression on the brachial plexus or pain that limits motion or inhibition of muscles in the area, but why would a person lose passive ROM in all directions?
Raul_SJ
G.O.A.T.
Yowzers! All 3 points hurt on me with the coracoid the worst.
I take it that you do not have frozen shoulder.
But this test claims 96% sensitivity and 87% specificity. Meaning that 96% of those with frozen shoulder will test positive and 87% of those without frozen shoulder will test negative.
Is this test worthless?
I take it that you do not have frozen shoulder.
But this test claims 96% sensitivity and 87% specificity. Meaning that 96% of those with frozen shoulder will test positive and 87% of those without frozen shoulder will test negative.
Is this test worthless?
I do not have frozen shoulder.
The test is not worthless. But remember, it's just one piece of the puzzle. Clinicians use provocative/special tests to further come up with a differential diagnosis along with other pieces of information that they've obtained during their evaluation.
I just wouldn't want someone who's lost some ROM and do this test to self diagnose themselves with having frozen shoulder. Then who knows what they'll do to self treat.
I think the only true way to diagnose true frozen shoulder would be to anesthetize the patient or the shoulder using a nerve block and see if the arm loosens up. In my case, the gradual onset also kind of signals true frozen shoulder. Also, when I do the pendulum where the arm is totally loose, noodle like, when I send the arm into a clockwise motion and let it do its thing I notice the interference from around 1 oclock to 5 oclock. This is with the arm dangling and my muscles just initiating a circular movement.
Similar threads
- Replies
- 3
- Views
- 735
